From Districts to Trusts
A
health care system, any health care system, is in a state of permanent
reform. I understand that annoys and upsets everybody who works in it. But it
is almost inevitable.
Kenneth Clarke in The Wisdom of the Crowd, 2013 25
The
period from the 1982 restructuring, through the Andrew Lansley reforms of
2012/3, saw a slow, progressive but massive change in the NHS. Secretaries of
State grappled with the problem of how to combine the central responsibility to
Parliament for a health service, with the need for devolution of decision
making. Financially there were intermittent crises. Socially, greater
patient/customer responsiveness was required. Clinically, until in
2020 the service was near overwhelmed by Covid-19, it was moving
from acute episodic diseases to the treatment of multiple chronic illnesses. The
development of magnetic resonance and other forms of imaging, new
pharmaceuticals increasingly based on genetic developments, rapid improvement in
cardiac surgery, in minimal access surgery and in day care changed the hospital
service. In general practice, family doctors gave up
their 24-hour responsibility and considered the way in which they might
cooperate across practices. Care in the community and integration of health and
social services were thought to provide a solution.
In
1982 the hierarchy of the NHS was clear and strict, a planning system
underpinned financial allocations and, in London as throughout
England, organisation was the same, if not in the other countries of the UK. By
2016 financial flows had changed, with the introduction of commissioning, and
care was delivered by a wide variety of trusts, some foundation ones with
greater freedom, but also by private organisations holding contracts. Indeed
whole hospitals might have been designed, built and partly managed by the
private sector, perhaps under the private finance initiative (PFI). People
received care paid for by the NHS; who provided it became less important both to
Labour and the Conservatives. Yet at the same time, quality and outcomes of
care had achieved an importance never previously seen.
From 2006 London had, for the first time, a single strategic authority, NHS
London. When abolished in 2013, London had its own NHS England region,
one of four. Instability had been consciously introduced. New styles of
management were called for and, as the market swerved between collaboration and
competition, new forms of regulation were needed partly driven by scandals.
Politically, the earlier years were dominated by the Conservatives, then for
over a decade by Labour, then a coalition of Conservatives and Liberal Democrats
and finally a Conservative administration once more. Nationally the economy
expanded in the early eighties, but in 1989 there was a recession after
Britain’s forced departure from the Exchange Rate Mechanism. By
the mid-nineties, the economy was once more healthy, and from 2000-2008 there
was an unprecedented increase in money for the NHS until in 2007
a worldwide financial recession brought growth to an end, and in spite strenuous
efforts, the majority of trusts were in deficit.
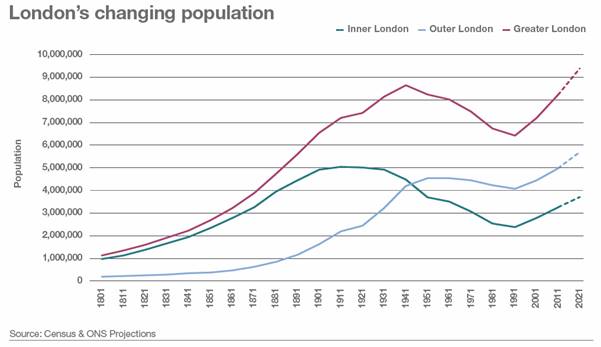
Demography
London's population was changing substantially in numbers, distribution, and
characteristics.1 From a peak of 8.6 million residents in 1939, it
fell for half a century to a low point of 6.73 million in 1988, its size 80
years earlier. After 1981 inner London grew more rapidly than outer London and
faster than the UK as a whole. By 2031 the population was expected to reach 8.8
million. In most of England the population was ageing, but in London it was
getting bigger and younger, with an increasing birth rate and a net inflow of
young adults. Docklands and the Light Railway, and building in Stratford for
the 2012 Olympics spurred regeneration in the east. There was an influx of
people from Eastern Europe as the European Community expanded. Soon the
indigenous population of London would become a minority.
|
Inner
London (millions |
Outer
London (millions) |
All
London (millions) |
|
|
1901 |
4.9 |
1.6 |
6.5 |
|
1939 |
8.6
(peak) |
||
|
1961 |
3.481 |
4.496 |
7.977 |
|
1971 |
3.060 |
4.470 |
7.529 |
|
1981 |
2.55 |
4.244 |
6.806 |
|
1991 |
2.599 |
4.23 |
6.829 |
|
2001 |
2.867 |
4.565 |
7.336 |
|
2006 |
2.954 |
4.508 |
7.559 |
|
2031 |
3.687 |
5,152 |
8.840 |
NHS
structural change
Continuous structural changes took place nationally. Key dates were
1982 Restructuring increasing district power and simplifying the planning
system
1989 Working for Patients; Conservative NHS Reform, splitting
commissioning and provision
1997 Labour’s The New NHS, Modern, Dependable, followed by a further
wave of structural change in 2000
2013 Lansley/Coalition structural changes abolishing Special Health
Authorities and producing disastrous confusion, gradually mitigated without
further legislation.
London reports.
Against the changing national background, London's services were regularly
reviewed. There was a new accent on quality, regional specialties, and primary
care, presaged by the reports of the London Health Planning Consortium. A
series of London reports, (1992 - Tomlinson 3, 1997 - Turnberg 4 and
2007 - Darzi 19) aimed for a hospital service that was smaller,
stronger and with a more substantial research base and better
infrastructure. Medical schools united, and health service mergers generally
mirrored them. In multiple reorganisations District Health Authorities
disappeared. Regional Health Authorities went as did their successor Strategic
Health Authorities. Consortia of commissioners, the London regional branch of
NHS England, and new Academic Health Science Centres replaces them as drivers of
change. Of the five UK Academic Health Science Centres identified three were in
London.
The
initial perception was that there were too many beds and too many small
specialist units, with only a small throughput of cases probably associated with
poor results. There was certainly a dearth of services in the long term sector,
for the mentally ill and the elderly. To the imperative of keeping within
budgets was added a new pressure for quality of care, fuelled by scandals of
poor care.
Underpinning the changes for much of the decade was the belief that competition
was to be welcomed, not feared, and that incentives might deliver better
performance. Change was driven by the financial climate, politically
inspired organisational restructuring and the belief that patient choice was
important.
Historically London's hospitals had ignored general practice. London seemed
unique in its failure to resolve the problems. The mobile young, a multitude of
ethnic and immigrant groups, an intelligentsia and users of drugs and alcohol
all congregated in London. Academic general practice developed late in London,
there were fewer innovative GPs and modern premises were less often to be
found. High land values, unsavoury locations and planning problems made it
almost impossible to find a good site in the right place. Recruiting young
doctors was a perennial problem. Inner city GPs were, on average, older, often
single-handed and many had trained overseas. Young doctors seldom wished to
enter such practices. ‘Better’ doctors went to greener pastures.
It
became received wisdom, without much supporting evidence, that substantial parts
of care delivered in hospital could be moved into the community. In a report
(Primary Health Care in Inner London, 1981 11) commissioned by
the London Health Planning Consortium, Donald Acheson, later Chief Medical
Officer, had provided an analysis of the problems. After the Acheson Report, it
was no longer possible to discuss health services in London without taking note
of the condition of primary care and making at least a symbolic gesture towards
the solutions of its problems. Brian Jarman wrote later than none of the
report's London-specific recommendations had been effectively
implemented. Following Acheson, attempts to improve matters included a London
Initiative Zone established after the Tomlinson Report to improve GPs' premises,
recruit a new cadre of GPs, introduce innovative approaches to old problems and
develop cost-effective care outside hospital. A review five years later showed
improvement in premises but in some areas the standards remained unacceptably
low. London still had fewer young GPs, more single-handed practices, and larger
lists. There were more practice nurses, but although primary care in the capital
was improving, it was doing so no more rapidly than elsewhere. The initiative
was terminated. The Turnberg Report (1997) again recommended support for GPs
and the need to improve recruitment and retention. It could be argued that the
pattern of general practice that worked excellently elsewhere was unsuitable for
inner cities and an alternative contract for GPs was introduced. "Personal
Medical Services" made salaried service practicable and seemed particularly
appropriate for London. After 2000, new national initiatives aimed to improve
access to the NHS, for example, walk-in centres - which were not particularly
successful. Urgent care centres were established alongside hospital A and E
units to filter off those not requiring the mostintensive facilities. The
importance of primary health care was stressed again by Darzi 19 (2007),
who wished to see the development of 150 large polyclinics from which all GPs
and the associated staff would work. In many areas, there were already plans to
provide better and larger premises, and these initiatives were promptly renamed
polyclinics.
In
general practice, family doctors gave up their 24-hour responsibility, throwing
extra strains on the hospital service, and considered the way in which they
might cooperate across practices, establishing clinical networks or federations.
Boundaries have always been significant in London hospital planning. If
hospitals were to be part of a system, they either had to be looked at in groups
or else in terms of the specialist services that they provided. Over the years
there have been discussions about whether London's hospitals should be
considered on a concentric or a radial pattern. The doughnut (with all the jam
in the middle) placed emphasis on the teaching and specialisationin the centre,
leaving the periphery alone. The alternative, the starfish (which had radial
communications and relationships), tried to relate central expertise to the
surrounding shire counties. In the late 1970s, the London Health Planning
Consortium had planned on a London-wide basis, although the implementation had
been left to the four Thames Regional Health Authorities and most took little
action. Rationalisation increased in tempo after the 1982 restructuring of the
NHS, spurred by financial pressures. After the demise of the London Health
Planning Consortium, the chairmen of the twelve teaching districts examined what
was happening and found it impossible to predict the future.
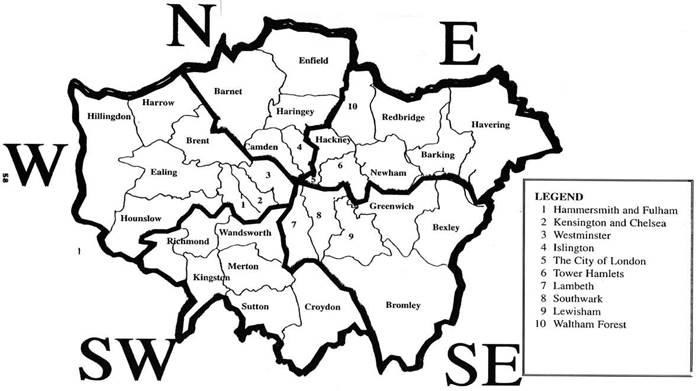
The spatial
framework of planning in London often changed, confusing and delaying
action. Sometimes the boundaries of the 4 Thames regions were used (1948 -
1994). Then there were Department regional offices (1996-2002). A five sector
scheme proposed by the Turnberg report (1997) was used, reflected in five London
SHAs (2002-2006) - North West London, North Central London, North East London,
South East London, and South West London. The five were reduced to two and then
a London-wide Strategic Health Authority (NHS London, July 2006) was introduced,
to be abolished by the Lansley reforms in 2013 in favour of a London regional
branch of the new NHS England. This appeared to follow the Turnberg five sector
approach.
National organisational changes and their London effects
1982-9 Conservative government & Working for Patients
The
General Management Function 5
NHS
management changed after a major review in 1983 by Sir Roy Griffiths, an outcome
of the industrial action of 1982 and the weakness of the 1974 restructuring. In
a memorable sentence he said, ‘if Florence Nightingalewas carrying her lamp
through the corridors of the NHS today, she would almost certainly be searching
for the people in charge.' Griffiths' recommendations included a small, strong
general management board in Whitehall, that all day-to-day decisions should be
taken in the main hospitals and clinicians should be involved more closely in
management decisions and should have a management budget and administrative
support. A general manager should be identified (regardless of discipline) at
each level and authorities should have greater freedom to organise the
management structure suited to their needs. Griffiths believed that the lack of
a clearly defined general management function was responsible for many problems
and that the development of management budgets was vital. Consensus had to go.
The government accepted the report.
1989 Working for Patients
6
The next major
organizational change took place under Mrs Thatcher and Kenneth Clarke. In 1986
twelve London hospital consultants wrote to the Times talking of the reduced
allocations and falling bed numbers.
"The inner
London population is no longer receiving an adequate medical service. The
future of the hospital medical service in London looks grim."
There were
demands for a review of the hospital and health service. What the professions
got, the Conservative's NHS Reforms, was not that for which they had been
hoping. Many of its concepts were later accepted by Labour. The basic NHS
structure had not altered greatly either during reorganisation of 1974 or
restructuring in 1982. The Conservative government repudiated consensus and
partnership with the professions in policy making, and the broadly bipartisan
approach to the NHS had ended. Among its beliefs were the importance of a sound
economy without which public services could not be funded; the view that there
was little the public sector could do that the private sector could not do
better; and that managerial inefficiency was rife throughout the public sector.
This approach was only part of a wider ideological battle about society,
industry and public services. The main ideas often attributed to Enthoven’s
Reflections on the management of the NHS, 7 were current in
radical-right circles. Working for Patients accepted many basic
principles of the NHS, central funding from taxation and largely free at the
point of usage. The idea that a major injection of funds was all that was needed
was rejected. Instead, reforming incentives and the introduction of a ‘market’
would improve productivity. The purchasing function would be separated from the
provision of services. Health authorities would concentrate on the assessment of
needs and contract for services; hospitals and trusts would provide them. A
good performance would be rewarded for money would follow the patients. The high
costs of central London, compared with the lower ones of hospitals on the
periphery, might be a problem for central hospitals.
Hospitals and
community services could apply for self-governing status. NHS hospitals were
progressively transformed into publicly owned substantially self-governing
trusts. Managerially élite hospitals had substantial freedom. The idea of
trusts had been developed with acute hospitals in mind, but applications were
received from mental illness and community services. They too saw advantages in
the freedom of action.
The
Trusts generated their revenue from contracts with districts, commissioning
agencies and GP fundholders. They needed good financial information, but the
data required to compare relative costs were poor; the necessary systems were
not in place. Many hospitals had no price list. Block contracts,
notional costs, and wild price variations were commonplace. It took much work to
sort things out. Over the first few years, there was some change in the
pattern of patient flows which had a potential to destabilise budgets, perhaps
5-10%. There had been anxiety that district purchasers would make more radical
changes, building up services in local hospitals many of which were new with
young staff and spare capacity, so avoiding high-cost hospitals in
the centre. The countervailing advantage in the centre was that a high
proportion of the medical and surgical consultants had sub-specialty expertise
making them the natural place for junior medical training.
Doctors were now employed by the trust and not the RHA, so they began to think
in a more local way. At Guy's, a hospital that had major financial problems but
wished to expand its services, clinical directorates were established under
medical control on the ‘Johns Hopkins’ model. Decisions could be taken more
rapidly, new patterns of staffing could be introduced, and services could be
improved without bureaucratic delays. Because their unit budgets were determined
by contracts with purchasers, it was easier to persuade consultants to change
their patterns of work.
The
need for hospital trusts to generate income led to visible changes.
Lilac coloured carpeting and easy chairs, smiling receptionists, a florist’s
stall bursting with blooms, a bistro coffee bar and newsagents would appear.
Trusts spent money on glossy pamphlets on their services, and logos. Acute
hospital trusts established private patient units to compete with private
hospitals and sometimes developed outreach services; community trusts looked at
hospital-type day care. The borders could blur. The boundary between the NHS and
private medicine was indistinct and the phrase ‘internal market’ seemed
increasingly inappropriate.
London Reports
There were two major planning exercises in early 1992, one by the King’s Fund
led by Virginia Beardshaw and one later that year initiated by
the government (Tomlinson 3).
1991
- The King’s Fund Commission 16
The
King’s Fund appointed a Commission in 1991 to develop a vision of services that
would make sense in the next ten years. RAWP was having a detrimental effect on
London, the RHAs were not taking a London-wide view, and there were fears that
the newly introduced internal market would disadvantage London’s hospitals. It
spent £500,000 commissioning 12 research reports and the final
document analysed the interlocking set of problems posed by health services,
medical education and research in London. It said that Londoners received a
poor deal and warned that health care in the inner-city might become
inappropriate unless there was the political will to back a strategy of
fundamental reform. The report accepted the case for a reduction in acute
services with a complementary build-up of primary health care, but did not
consider the paucity of back-up beds in nursing and residential homes that
barely existed in the metropolis. It reported that at least 5,000 beds must be
closed if the capital were to be guaranteed a good standard of health into the
next century. ‘Costs in London are not just expensive, they are extremely
expensive . . . change is inevitable . . . Inner London hospitals are top-heavy
with doctors and the rate of patients going through is slower.' While the
report indicated the direction of change needed, it did not suggest the choices
that had to be made or which sites might be closed. Attacks were mounted on its
findings because of a belief that it was working towards a pre-determined
conclusion and that some of its members had little sympathy for London or for
specialists. Virginia Bottomley, Secretary of State from April 1992 to July
1995, would have liked support for decisions she needed to take. She did not get
it.
The
Conservatives, committed to market solutions but faced with clear problems
requiring decisions, embarked on strategic planning. At the 1991 Conservative
Party conference William Waldegrave, then Secretary of State for Health,
announced a review by Sir Bernard Tomlinson, Chairman of the Northern RHA. A
safe pair of hands, he would ensure that the King's Fund did not 'run away with
the ball.' Big building projects were imminent at UCH and St Mary's and there
was no logical basis for making decisions. The Times said
that Mr Waldegrave was ‘wringing his hands’ over what should be done and needed
to be convinced that major decisions were intellectually based.
UCH/Middlesex, strongly supported by the scientific community because of the
quality of its work, wanted a new building and this might mean the closure of
other hospitals. Already expansion had been approved at Guy’s, the Chelsea and
Westminster was established and St Mary’s was being developed. The effects of
RAWP on central hospitals, in the event over-estimated, and of the internal
market, were key to the commissioning of the inquiry. However, William
Waldegrave had delayed the need to take action before an election. Those working
on the two reviews cooperated, and data was exchanged.
Tomlinson reported in October 1992.3 He emphasized
the need to improve primary and community care to national standards
and provide services for people with special needs such as the
homeless. Tomlinson argued for this, and the government provided £170 million
over six years in a ‘London Initiatives Zone’ covering about 4 million people,
where needs were great, and an innovative approach was required. Most
people under-estimated the complexities of building new and better facilities
for GPs and primary health care teams. Neither was it easy to turn a
theoretically attractive plan for the teaching hospitals and medical schools
into schemes on the ground. The money helped new projects and encouraged the
study of long-standing problems of inner London practice but the p Tomlinson
reported in October 1992.3 He emphasized the need
to improve primary and community care to national standards and provide services
for people with special needs such as the homeless. Tomlinson argued
for this and the government provided £170 million over six years in a ‘London
Initiatives Zone’ covering about 4 million people, where needs were great and an
innovative approach was required. Most people underestimated the complexities of
building new and better facilities for GPs and primary health care teams.
Neither was it easy to turn a theoretically attractive plan for the teaching
hospitals and medical schools into schemes on the ground. The money helped new
projects and encouraged the study of long-standing problems of inner London
practice but the pace of change was slow and the effect on acute hospital
services minimal.
The
Tomlinson Report foresaw a surplus of 4-5,000 beds because of the withdrawal of
inpatient flows from outside central London and the increasing efficiency with
which beds were used. The report suggested reducing the number of medical
students in London by 150. Whole hospitals should be taken out of use and the
resources redeployed to develop primary care and community services. Tomlinson
revived earlier proposals forrationalisation. UCH/Middlesex that had
become a single, powerful and scientifically
important organisation. The Middlesex site of the combined University
College/Middlesex hospitals should close and its services relocated tothe
University College Hospital site. The London Hospital for Tropical Diseases, and
the Royal National Throat, Nose and Ear, at Gray's Inn Road, would shut, and
move to the redeveloped University College Hospital There would be a single
management unit for St Bartholomew’s and The Royal London; the loss of one
hospital from among the south London hospitals of Guys’, King’s, St Thomas’ and
Lewisham, and Guy's and St Thomas's should merge on one site. The report
proposed linking 8 of the 9 London medical schools into four and associating
them with four multi-faculty colleges of the University.
The
Homerton in Hackney should take most Hackney patients currently treated at
Bart's. The Middlesex site of the combined University College/Middlesex
hospitals should close and its services relocated on the University College
Hospital site. The London Hospital for Tropical Diseases, and the Royal National
Throat, Nose, and Ear, at Gray's Inn Road, would shut, and move to the
redeveloped University College Hospital. Guy's, by London Bridge station, and
St Thomas's, a mile away opposite the Palace of Westminster should merge on one
site under a joint trust board. St Mark's Hospital, in Islington, which
specialised in the treatment of bowel diseases, would become part of the
Northwick Park district hospital complex in Harrow, Middlesex.
Charing Cross, in Hammersmith, which had the greatest excess costs, must close.
The Royal Brompton hospitals, dealing with heart and lung complaints, and the
Royal Marsden cancer hospital should be brought together on the vacated Charing
Cross site. If not, the site should be sold. St Mary's, Paddington needed to
reduce the number of its beds, and Queen Charlotte's maternity hospital
should shut, and its services moved to the Hammersmith. The capital's
postgraduate research institutions should consider ways to concentrate the
single specialty research institutes on fewer sites.
Sir
Bernard estimated that cuts in acute services and rationalisation could yield
£54m a year. There were four broad responses: the optimistic that primary and
community care could be brought up to the standards elsewhere; the realistic
accepting the recipe but gloomy about the money and the difficulties; the
despairing who doubted whether anything would be accomplished; and the reaction
at St Bartholomew’s that was to indulge in old-style emotional campaigning
against the proposals. St Bartholomew’s had come to believe its
own rhetoric, and dismissed any proposal not to its liking, however well
founded. Its campaign was given a voice by the Evening Standard in
probably the most ferocious media war ever waged against health service managers
and NHS policy, unparalleled in its unstinting aggression and partiality.
After the
unexpected Conservative victory in April 1992, the new Secretary of State
Virginia Bottomley began to take decisions although eminent men tried to bully
her. "I had all these great-uncles who died in the first war, we were taught
that when the whistle blows you get out of the trench and you walk towards the
guns. That is what I was brought up to do, to get out of the trench and walk
towards the guns."3 She redefined the NHS as the provision the
provision of care on the basis of clinical need, regardless of the ability to
pay, not by who provided the service. In February 1993 the Department of
Health's response Making London Better, 3 accepted the general
thrust of the recommendations, and the need to develop primary health care. It
provided a comprehensive blueprint for further development, some of the changes
ultimately proceeding. (*)
UNIVERSITY COLLEGE/MIDDLESEX: The hospitals should merge on one site and absorb
two of the smaller specialist hospitals, the Royal National Throat, Nose and
Ear, and the Hospital for Tropical Diseases. (*)
ST
BARTHOLOMEW'S: appraise three options - closure, merger with the Royal London
and the London Chest; or retention as a smaller specialist hospital (*)
ST
THOMAS'S and GUY'S: Merger consolidating services on one site
CHARING CROSS: A&E workload to transfer to the new Westminster and Chelsea
hospital. (*)
ROYAL BROMPTON and ROYAL MARSDEN: consider merger. Perhaps their institutes,
could form part of a new Chelsea Health Sciences Centre
QUEEN ELIZABETH: merge with the nearby Homerton (*)
ST
MARK'S: move to Northwick Park (*)
To
drive the implementation of the Tomlinson proposals, a London Implementation
Group (LIG) was formed, chaired by Tim Chessells, Chairman of North East Thames
RHA, who had direct access to Ministers. Six specialty reviews were established
to examine clinical requirements; the clinicians in the specialty under
consideration came from outside London and could be brutal when faced with the
pretensions they sometimes encountered. The reviews (1993) proposed that the
best centres should be developed, the smaller ones should be closed or merged,
and new ones established where they were needed as at St George’s where there
was a long-standing need for renal replacement therapy. Many of the
recommendations were implemented; too much was expected too fast. Some were
revised as a result of more general considerations, e.g. in
the south-east neurosurgery was not maintained at Guy's but at the
Maudsley. Several initiatives now came together making change possible. A
research review of the London postgraduate hospitals pointed to the need for a
wide range of skills including biophysics and molecular biology, and association
with general hospitals and university facilities. Medical school deans had to
play a difficult hand; most were privately supportive of the need for change and
prepared to work for it, but in public they had to take their colleagues with
them as far as possible. Trust chairmen had been appointed knowing there was a
job to be done. They and their chief executives were heavyweights who did not
fool around, and transitional funds were available to sugar the pills of change
and mergers. Ministers were far more involved than they had been in the work of
the LHPC. The Higher Education Funding Council (HEFCE), as a member of the
London Implementation Group, was involved in medical school mergers and
amalgamations, as well as through its direct links with the institutions. The
London Implementation Group closed down in April 1995, and the then two Thames
RHAs north and south of the river became responsible for co-ordinating change,
though they too were facing demise.
Guy's was in a difficult position. It had been lauded as a "Flagship" NHS
Trust, but in 1991 a black hole appeared in its finances damaging its
record. Tomlinson had suggested a merger on one site with St Thomas's, but
which site? A vicious feud broke out, the Chairman and Chief Executive of Guy's
were replaced, and their successors argued successfully for managerial
integration but a two-site solution. Guy's increasingly became the major
academic location with regional specialty work, and St Thomas's the acute
hospital with accident and emergency. In parallel, the United Medical and
Dental schools battled with academic integration. ‘During the past twenty
years,’ wrote Lord Flowers in The Times, ‘with a
few honourable exceptions every attempt to reform London medicine has been
defeated by vigorous rear-guard action on behalf of any hospital or medical
school adversely affected. The result has been that the standing of teaching and
research in London’s famed medical schools has been steadily slipping. The time
has come for the government to stand firm.’ In Making London Better 3,
Virginia Bottomley took decisions that her predecessors had been canny enough to
defer and for which her successors would be forever in her debt; she was
prepared to bell the cat, as the BMJ had put it. She narrowly escaped
defeat in Parliament and a rebellion of some senior London Tory MPs. Her reward
was the Department of National Heritage. Robert Maxwell, Secretary of the King’s
Fund, said that the creation of big medical centres across London, the main
tertiary centres of service, research and education for the future, had been
talked about for 50 years. Now it looked set to happen and would
be Mrs Bottomley’s best legacy.
Industry had been removing middle management, ‘downsizing’ and producing ‘flatter’ organisations but few foresaw that regions might be abolished. A review in 1993 of the relationship of the 14 RHAs with the centre recommended that regions should be amalgamated into eight in April 1994. London was divided in 1996 into two regions, north and south of the river. Finally regions were abolished in favour of eight regional offices of the Department of Health.
1997 - The Labour government
The
new NHS - Modern, Dependable 9
Labour took power in 1997 and Frank Dobson, the new Secretary of State, set out
Labour's initial vision in The New NHS - Modern, Dependable. The harder
edges of the internal market were softened. Fund-holding went, co-operation
replacing more extreme forms of competition. The interdependence of health and
social care, and joint programmes, were stressed. In June 1998 Frank Dobson,
decided that London would form a single NHS region and a single London Regional
Office of the NHS Executive was established in January 1999. The arguments
against such a pattern, vetoed by Bevan in 1946 and also rejected at the time of
the 1974 NHS reorganisation, were now weaker. A London region had been proposed
by Tomlinson. Change had therefore been expected and affected the boundaries of
the surrounding areas. Hospital trusts became accountable to regional
offices for their statutory duties, and to health authorities and later primary
care trusts for the services they delivered. The separation of planning from
provision and decentralization of hospital management was maintained. If
Tomlinson had been the Conservatives’ review of London, Turnberg was Labour’s.
1997 – Turnberg 4 The NHS and University Medical Schools
Until the mid-1990s it was believed that London's hospitals provided too many
acute beds and it was right to reduce their number. As London came under ever
increasing financial pressure following the Resource Allocation Working Party
Report (1976), and clinical developments speeded earlier discharge, hospitals
were closed against substantial opposition and the number of beds continued to
fall. 'Every workhouse I tried to close,' said Kenneth Clarke, 'was regarded as
a centre of clinical excellence by all the staff who worked there and all its
patrons. The most extraordinary dumps were defended by banner-waving
demonstrators.'25 Ultimately the belief that there were too
many beds became untenable. After the election Labour had faced problems with
commitments such as no hospital closures - Frank Dobson had made scurrilous
remarks about Virginia Bottomley's decisions on St Bartholomew's - an end to a
postcode lottery and the salvation of St Bartholomew's. Labour saw that health
services needed to be coordinated with changes in medical education and, perhaps
to get himself off the hook, Frank Dobson commissioned a strategic review of
inner London, increasing uncertainty just as some clarity had been obtained. Led
by Professor Sir Lesley Turnberg, it reported within months.4 It
focussed on wider strategy, recommending large scale planning for major change,
greater involvement of the public in the development of proposals and a future
focus on primary and community care. It made specific recommendations in
relation to several hospital sites. It was clear that there was great pressure
on London services, workload was rising and the number of GPs was falling.
Hospital bed numbers had fallen substantially; between 1990/1 and 1995/6 1130
acute inpatient beds had disappeared from inner London, and when geriatric,
maternity and psychiatric beds were included the loss across London as a whole
had been 9,271. Turnberg concluded that there was now no evidence that there
were more acute beds available to Londoners than the English average, taking
into account the use of London beds by non-Londoners. The subsequent NHS Plan (2000)10 accepted
that a substantial increase in capacity was needed if waiting lists were ever to
be reduced. Improvements in primary care had not been able to substitute for
reductions in secondary care. The campaigning by St Bartholomew's gave an
impression that its fate was the key decision Turnberg took, but the Royal
London Hospital was planning a massive rebuild and other important issues
included mental illness, primary care and community services, and the medical
school mergers that had health service consequences. Queen Mary's Roehampton was
also scheduled for closure.
Turnberg felt that a five sector scheme would assist planning and health
authorities should work together at sectoral level. This scenario has had a
permanent effect on health planning in London. The sectors were not unlike the
inner parts of the old Regional Health Authorities (for the shire counties had
been separated) and reflected a five sector scheme Tomlinson also had
liked. Radial organisation had been referred to in the sixties as a "starfish"
pattern. The more egalitarian term of Pizza slices was now used and within the
slices PCTs, Trusts and the educational authorities had a commonality of
interest that led them to work with each other, rather than with other slices.
Reconfiguration
A
new imperative was now emerging - rationalising/reconfiguring the hospital
system. The need to provide specialised expertise 24/7, medical staffing
problems and the restriction of the hours worked under EC legislation had
changed the criteria for defining the size a safe hospital. The progressive
increase of sub-specialties meant that rotas of consultants in all the
subspecialties could be accommodated in a large hospital but not in smaller
District General Hospitals (DGHs). Now that far more specialties were involved
in care, there had to be full cover of each to provide a 24-hour service. It was
rational to plan for fewer major hospitals, strategically placed. These might be
supported by more local facilities. National Service Frameworks developed for
clinical specialties outlined clinical networks of hospitals varying in their
sophistication. Reports of the BMA, Royal College of Physicians (RCP) and Royal
College of Surgeons of England echoed the earlier thinking of the Bonham-Carter
Report (1969), suggesting that a single general hospital now should serve
populations of not less 500,000.14 Under pressure
to improve the volume and quality of services without higher costs, some trusts,
for example the Central Middlesex, introduced process re-engineering. If the
stages in the delivery of care were examined, was there a better way of
designing the system? Given better drugs and anaesthetics allowing more speedy
recovery, state-of-the-art diagnostics and imaging, minimum intervention
techniques and better information systems, could any stages be omitted, or be
arranged more economically to save the time and money of both patients and
staff? When financial pressures grew, and problems of quality emerged, trusts
increasingly considered that merger would help to solve problems. Progressively
these took place.
A
related problem was the provision of effective emergency care when most
consultants were super-specialists. The RCP said half of the hospitals it
surveyed had adopted an emergency admission ward, perhaps of 20 beds, with a
system of assigning patients to specialist units. The RCP suggested that Acute
Medicine was a separate specialty, required by each hospital taking acute
admissions.
Hospital developent in the five Turnberg sectors
New hospitals planned in the 1970s had opened in the 1980s, for example, the Newham Hospital (1983) and the Homerton in Hackney (1986). Development was often supported by the Private Finance Initiative (PFI), and major changes took place in each of the five 'Turnberg' sectors adopted as the boundaries for managerial bodies. The problems with PFI were the inflexibility once the building had been opened and the financial costs that stretched way into the future and sometimes closed off other opportunities.
From 2002 until
2006 London had five Strategic Health Authorities and from then until 2012 a
single one, NHS London, with an overview of the entire metropolis.
North East London
In the North East
decisions were most needed about The Royal London and St Bartholomew's, Queen
Mary College and the medical schools of the two hospitals. These two hospitals
and their staff had long-standingdivergences and a deep distrust of each
other. As part of the Conservatives' NHS reforms (1990), the idea of
self-governing hospital trusts within the NHS was introduced, and Bart’s was
planning to set up such a Trust when its independent future was called into
question by the Tomlinson Report which did not see Bart’s as a viable hospital
and recommended its closure. The Government’s response in 1993 supporting
Tomlinson gave three options for Bart’s: closure, retention as a small
specialist hospital, or merger with the Royal London Hospital and the London
Chest Hospital. This sparked an intense public debate and a campaign to save the
hospital on its Smithfield site. In April 1994 a Trust was formed,
incorporating the three hospitals. Turnberg had supported the case for
the redevelopment of a 900 bed secondary and tertiary care hospital
in Whitechapel while maintaining some tertiary services at Smithfield, mainly
cardiac and cancer services. A billion pound PFI development began, the
financial cost of which overhung the trust and prevented it achieving foundation
trust status. Later mergers were encouraged, culminating in 2012 in the creation
of a huge trust, Barts Health, uniting St Bartholomew's, The Royal London,
Newham and Whipps Cross hospitals. Its management insisted that major savings
could be made, but they proved illusory. By 2015 there was an annual
deficit of £93 million, a CQC report revealed poor nursing standards
particularly at Whipps, and the trust was put into special measures. An
agreement was made with UCLH to exchange cardiac services for cancer, leaving
Barts to concentrate on the former.
New building was
undertaken at Whipps Cross and Newham General (an Ambulatory Care and
Diagnostics Unit and an adult mental illness unit). A new Queen’s Hospital in
Romford brought together the services previously run at Oldchurch and Harold
Wood hospitals; built under the Private Finance Initiative, it opened in 2006,
complementing the rebuilt St George's Hospital Ilford where lower risk
and midwife-led maternity care was provided. It was the second of two huge
hospitals in north-east London.
North Central London
The
Department of Health had supported merger discussion between the medical schools
of UCH and the Middlesex Hospital, two organisations with a similar ethos, and
the previous boundary between North East Thames and North West Thames was moved
so that the districts containing these hospitals united in 1982 as Bloomsbury.
The Eastman Dental Hospital had special health authority status but in 1996
joined UCLH. The Elizabeth Garrett Anderson Hospital (1888) became part of UCLH
in 1994. The Hospital for Tropical Diseases, the home for the London School of
Tropical Medicine, moved first to St Pancras Hospital and then to the main part
UCLH. The National Hospital for Neurology and Neurosurgery joined in 1996, the
Institute of Neurology affiliating to UCL. The Royal London Homeopathic Hospital
joined the group in April 2002.
Turnberg supported the proposal for capital development and ground was broken in 1999 for a £422 million private finance initiative that opened in 2005 uniting most of the University College London Hospitals on a single site. The old Middlesex Hospital site was sold off profitably for redevelopment as flats, gaining the Trust £175 million. With its new development commissioned, and its financial situation sound, the Trust rebuilt its obstetric hospital (the EGA wing) and cancer unit and looked to bring other hospitals, including postgraduate teaching hospitals, onto its site, e.g. the transfer of the Royal National Throat Nose and Ear Hospital from The Royal Free to UCLH.
Substantial development was taking place elsewhere. The first phase of a new Barnet General Hospital opened in 1997. A major development took place at the Whittington. At Chase Farm Hospital, a new surgical wing and Treatment Centre was built, and the North Middlesex was redeveloped with a new Emergency Care Centre, Diagnostic and Treatment Centre, and an Acute and Critical Care Centre.
A world-class medical science centre for London was developed by a partnership of Britain’s biggest funders of clinical research, the Medical Research Council (MRC) National Institute for Medical Research, the Wellcome Trust, Cancer Research UK and University College, London (UCL). A £350 million scheme went forward on a 3½ acre site near the British Library and St Pancras station. The Francis Crick Institute was the largest laboratory of its kind in the world, accommodating 1,500 leading researchers in different fields In 2011 Kings College and Imperial signalled their intention to associate with it.
North West London
Centrally the sector contained the Hammersmith, Queen Charlotte’s, Chelsea Hospital for Women, Charing Cross and, nearby St Mary’s, the Chelsea and Westminster and two specialist hospitals, the Royal Marsden and the Royal Brompton. It came to be dominated by Imperial College. In 1984 the medical schools of Charing Cross and Westminster hospitals united, and in the next year, the districts in which they were situated were merged into one authority, Riverside District Health Authority, with plans to rebuild and reduce the number of hospitals to two. Brent and Paddington District Health Authorities 'huddled together for strength and warmth,’ in the words of the district manager. In 1988 Parkside Health Authority was created, uniting St Mary’s and the Central Middlesex, leaving St Charles’ as a non-acute community hospital. Hospital planning involved the part-rebuilding of St Mary’s and rebuilding the Central Middlesex, the first phase being a pioneering ambulatory care centre. The new Chelsea and Westminster Hospital, which enabled the closure of five separate hospitals, opened in 1993. The Hammersmith/Queen Charlotte's new maternity facility opened in 2003.
The Turnberg report called for more rational distribution of specialist services in North West London. The outcome was the Paddington Health Campus project, a variant of the proposals in the Pickering Report of the 1960s to be funded by PFI. It would bring together Royal Brompton & Harefield NHS Trust, St. Mary's NHS Trust, Imperial College's National Heart and Lung Institute and North West London’s specialist children's services to one site in Paddington. The Business Case was approved by the Department of Health in 2001, but the cost steadily escalated until it was clear that it was not viable. It was cancelled in 2005.
In
the early 1990s the Medical Research Council (MRC), under financial pressure,
decided to pull out of its Northwick Park Clinical Research Centre and
concentrate at the Hammersmith Hospital. Northwick Park had been bought by
Charing Cross Hospital in 1944 to allow it to relocate from the centre.
Ultimately it had became a colocation of research and a district general
hospital that had a "normal" case-mix. Perhaps the idea of this association was
flawed; science grafted into an unreceptive environment at a district general
hospital where there were suspicions that patents would be "experimented
upon.” Perhaps the decision was partly the result of forceful personalities and
power politics.
This withdrawal freed modern accommodation and research space. A small specialist hospital concerned with coloproctology, St Marks, needed to move from its poor accommodation in City Road. St Marks had the foresight torealise that it had more to lose than gain from a merger with Barts and grasped the alternative, Northwick Park, with enthusiasm. Relocation in 1995 provided immediate access to intensive care, theatres and state-of-the-artimaging and service departments. St Marks had its own front door, clinical directorate and all the advantages of association with a busy district general hospital. Organisationally there was amalgamation within the North West London Hospitals NHS Trust incorporating Northwick Park & St Mark's and hospitals in Harrow, & the Central Middlesex.
The Royal Brompton & Harefield NHS Trust was established in April 1998 based on two sites, one in central London and one in Middlesex. The Trust provided services for all age groups from infancy to old age and associated with its multi-faculty university partner Imperial College School of Medicine within which was the National Heart and Lung Institute. Turnberg supported the approach to collaboration in the rationalization of services that was being undertaken by the hospital trusts and Imperial College. In 2007 under the aegis of Imperial College, it was proposed to bond the Hammersmith Hospital and St Mary's to create an Academic Health Sciences Centre, merging units such as renal medicine, and making it easier to bring cutting edge research earlier into clinical practice. This was accredited in March 2009.
In a
collaborative exercise, the eight CCGs took forward an earlier Darzi era
exercise, 'Shaping a healthier future' (2012) that aimed to
provide better care in the community. Its proposals to downgrade some A & E
Departments including Hammersmith and Charing Cross aroused opposition.
South West London
In south west London the position of St George’s was secure, and the plans to relocate the Atkinson Morley Hospital to the St George's site, and further developments there, were supported by Turnberg. The neuroscience and cardiac centre, the Atkinson Morley Wing, opened in October 2003
South East London
In
southeast London, Turnberg said that the merger of the Guys’ and St Thomas’ had
allowed the development of proposals for rationalizing services across the two
sites. There was protracted discussion and much in-fighting about the future,
whether one or the other site should close, where the accident and emergency
department should be situated, and where specialised services should be
concentrated. If these two hospitals agreed on anything, it was that King's
College Hospital was subordinate. Ultimately the A & E Department went to St.
Thomas’ because ambulance access was far better. There had also
been discussion about the distribution ofspecialised services between St
Thomas', Guy's and King's College Hospital. A new wing at King's College
Hospital opened in 2003, and a new Children's Unit was planned.
Turnberg examined redevelopment of acute services in Bexley and Greenwich, and supported the redevelopment of Queen Elizabeth Hospital to replace services at Greenwich, built under PFI at the cost of £93M. This involved the redevelopment of the former military hospital including the design, construction and financing of new buildings, the refurbishment of existing ones and the maintenance and operation of the entire hospital. Both it and Bromley soon had large deficits because of the irreducible costs of their whole hospital PFI schemes.
Since the time of the Royal Commission on Medical Education (1968) academic mergers had been proposed. The earlier Todd pairs differed substantially from the pattern later implemented.
|
St
Bartholomew's Medical College |
The
London Hospital Medical College |
Queen
Mary College |
|
University College Medical School |
Royal
Free Hospital School of Medicine |
University College |
|
St Mary's
Hospital Medical School |
Middlesex
Hospital Medical School |
|
|
Westminster Medical School |
Charing
Cross Hospital Medical School |
Imperial
College |
|
Guy's
Hospital Medical School |
King's
College Hospital Medical School |
King's
College |
|
St
Thomas's Hospital Medical School |
St
George's Hospital Medical School |
(Kingston) |
Todd pairs
St Bartholomew’s Medical College and The London Hospital Medical College;
University College Hospital Medical School with the Royal Free Hospital School of Medicine;
St Mary’s Hospital Medical School with the Middlesex Hospital Medical School;
Guy’s Hospital Medical School with King’s College Hospital Medical School;
Westminster Medical School with Charing Cross Hospital Medical School;
St Thomas’s Hospital Medical School with St George’s Hospital Medical School.
Final Mergers
Imperial College
Westminster Medical School
Charing Cross Hospital Medical School
St Mary's Hospital Medical School
Queen Mary College
St Bartholomew’s Medical College
The London Hospital Medical School;
Kings College
Guy's Hospital Medical School
King's College Hospital Medical School
St Thomas's Hospital Medical School
University College London Hospitals
University College
University College Medical School
Royal Free Hospital School of Medicine
Middlesex Hospital Medical School
St Georges
---------------------------------------------------------
Queen
Mary's
wished for a medical faculty, but was in a financially weak situation, as were
the two medical schools involved, St Bartholomew's and The Royal London. There
were substantial objections to amalgamation from both the medical schools, and
the merger in 1995 as Bart's and The London School of Medicine and Dentistry,
the medical faculty of Queen Mary University of London, was not a happy
one. Bart's and the Royal London had everything one could desire regarding a
local population, but the association with QMC, comparatively weak as a research
institution, did them no favours and the QMC and the two medical schools
associated with UCL Partners.
University College London
University College/Middlesex schools merged in 1987. The Institute of Child
Health became part of UCL in 1996 & the Royal Free and University College
Medical School was formed in 1998. University College London Hospitals while
having only small local catchments had substantial financial assets and an ideal
academic location next to UCL, perhaps the strongest research base in London. As
UCL Partners, it was selected as a National Biomedical Research Centre, in 2008
comprising UCL with Great Ormond Street, Moorfields Eye Hospital, The
Royal Free, and University College London Hospitals. New "partners" steadily
joined. As “London's leading health research powerhouse" it focussed on ten
areas of research which posed a major health challenge, e.g. children's health,
cancer and women's health. Though the medical schools merged, the Royal Free
Hospital remained under separate NHS management.
Imperial and UCL discussed a merger but decided it was in the interests of
neither side. However, the discussions divided the London medical schools into
two camps, Imperial College and UCL neither of which were supportive of the
concept of London University, and the other three. In 2005 UCL gained
independent degree-awarding powers from the Privy Council. Students registering
after 2007 had a UCL degree. Such moves, covering all subjects and not solely
medicine, tended to undermine London University.
Imperial College
Imperial College gained a medical school by merger with St Mary’s Medical School
in 1988. Its Faculty of Medicine was formed in 1997 by the merger of St Mary's
Medical School with Charing Cross and Westminster Medical School, the Royal
Postgraduate Medical School and the National Heart and Lung Institute. In 1988
the Royal Postgraduate Medical School had merged with the Institute of
Obstetrics & Gynaecology and also became part of the Imperial College School of
Medicine. The National Heart and Lung Institute situated next to the Royal
Brompton Hospital became part of Imperial College in 1995 and part of Imperial
College School of Medicine in 1997. Secure in its prestige and size, Imperial
took a firm line with the medical schools that were now an intrinsic part of it,
and with the hospitals to which they related. In 2007 St Mary's Hospital Trust,
The Hammersmith HospitalsTrust and Imperial College united to become the
Imperial College Health Care Trust, and this was selected as one of five
National Biomedical Research Centres. In 2003 it was given the power to award
its own degrees but did not immediately use it.
Imperial thought that globally there was only room for 5-6 major biomedical
research and teaching centres, perhaps two in the USA, one in the Far East and
two in Europe. Imperial considered itself the natural premier leaguecentre in
the UK. The Medical Faculty ethos was that of Imperial College, scientific based
and of the highest standard. There was a thorough reorganization to develop an
integrated Faculty, one organisation using the same letterheads The attempt to
bring the NHS and the academic side together as a single body did not work. The
huge problems of old buildings and financial deficits proved an excessive burden
on top management.
King's College
The
United Medical and Dental Schools (UMDS) of Guy's and St Thomas' was formed in
1982 and King's College London School of Medicine at Guy's, King's and St
Thomas' Hospital (earlier the GKT School) in April 1998. KCL, associated with
such powerful hospitals, gave UMDS room for manoeuvre. Internally there were
power struggles on both the service and the academic sides to determine the
future pattern of service. From 2007 students registered with King's were
awarded a King's degree, rather than one from the University of London. In
March 2009 King's Partners became accredited an Academic Health Sciences Centre
and made rapid progress to become a major player.
St
George’s
St
George's, far from the centre of London and with no substantial university link,
was not in the same league. It maintained an independent position within the
University of London but later established links with Kingston University
There were now four university centres, each related to a multi-faculty college,
plus St George’s. The postgraduate institutes were finally brought within the
fold, as proposed by Sir George Pickering in 1962.18 Within this
structure, once the colleges became directly funded by the Higher Education
Funding Council for England (the successor in 1993 to the University Funding
Council) the University of London had to accept the realities of local
ambitions, including the individual right to grant degrees. The colleges had
gained financial and managerial autonomy, UCL, Queen Mary, Kings and Imperial
being separately identified from 1993/4 and St George's two years later. The
University maintained a coordinating group of the medical faculties to discuss
strategy for mutual benefit but each college took a different approach to the
integration of medical schools within their fief.
The
replacement of Frank Dobson in 1999 as Secretary of State for Health by Alan
Milburn heralded further change. Milburn wished it to be fast and over a broad
front. Labour's second major health policy document, the NHS Plan, was
issued in July 200010 with four main themes, increasing
capacity, setting standards and targets, supervision of the way the NHS
delivered services, and 'partnership'. There was no specific London
agenda. Substantial progress was achieved in terms of waiting times and waiting
lists. Milburn’s policies involved a greater role for the private sector, for
example in the private finance initiative and independent treatment centres,
radical changes in funding with the introduction of tariffs and Payment by
Results, and Foundation Hospital Trusts with greater freedoms.
Trusts and Foundation Trusts (FTs)
In
July 2002 it was proposed that acute hospital trusts that had performed
well could apply to be "NHS foundation trusts". These would have greater
freedom in terms of management, closer links to their community and greater
local financial control. Authorisation as a FT was hard to obtain as the trust
had to meet high standards of financial security and governance
excellence. Nevertheless three London hospitals appeared in the first wave in
2004, Moorfields, the Royal Marsden and the Homerton. Later UCH, King's College
Hospital, the Royal Brompton and Harefield, and Guy's/St Thomas' also became
FTs. The Royal Free became one in 2011 and Kingston in 2012. Compared with the
rest of England fewer London hospitals became FTs. In many cases there were
financial problems, often relating to a debt overhang from developments under
the private finance initiative as in the case of the Royal London Hospital and
hospitals in South London. The trusts of the West Middlesex and Barnet/Chase
Farm sought association with existing FTs.
NHS
Foundation Trusts differed from existing NHS Trusts in key ways for they had the
freedom to decide at a local level how to meet their obligations; they were not
under the supervision of the special health authority; they had an individual
constitution that made them accountable to local people, who could become
members; and governors who could hold the board to account and, indeed, appoint
and sack the Chair
They were authorised and regulated by Monitor which kept a careful eye on
financial risks, and could provide new services and develop their facilities
from their own resources as they wished. For example, the Homerton successfully
bid to provide community nursing services to its area. If an FT sold land, it
could keep the proceeds for re-development. University College Hospital, also
an FT, sold the site of the old Middlesex Hospital for over £175 million, which
greatly assisted its redevelopment. Their revenue came largely from contracts
with the local ‘purchaser’ for which they competed with other trusts.
New patterns of hospital
medicine in London.
The NHS
Plan's structural reorganisation took place on 1
April 2002, "devolution day." At that point, there
were 28 Strategic Health Authorities.,with five for London. New
factors began to drive changes in hospital medicine in London, far more than
elsewhere. Increasingly services were planned across and between
hospitals and trusts, not merely within them. Services might be
provided more effectively in larger units, perhaps by hospital mergers
reflecting changes in the pattern of London medical schools, and there was a
drive to reconfigure services by clinical outcomes as in heart
disease, trauma and stroke
Organisational change continued in London. In 2004
Ministers said 'the unique nature and scale of health service issues facing the
capital might point to a single organisation to oversee service
development.' Following the Government report Commissioning a
Patient-led NHS (Department of Health, 2005), a single SHA was
established in London, though the PCTs that were largely coterminous with
boroughs were left unchanged.
NHS
London (SHA) and the Darzi Reports
NHS
London covered an area coterminous with the local government office region and
was established in July 2006. It was closed as a result of
the Health and Social Care Act 2012 on 31 March 2013. It brought together 5
SHAS, North West London, North Central London, North East London, South East
London, and South West London. It was, therefore, the
nearest that London had ever had to a "Central Hospital Board for London,"
providing strategic leadership for all of the health services in
the capital and with responsibility for the performance of 31 primary care
trusts. It had less responsibility for 16 self-governing
foundation trusts. NHS London was chaired in turn by George Greener, and after
his resignation in September 2008 by Sir Richard Sykes, previously chief
executive of GlaxoSmith-Kline. Sykes resigned as Chair in May
2010. NHS London had responsibility for those trusts that were not
Foundation trusts, for example, south London hospitals and Barts
and the London, which involved substantial firefighting, but also the formation
of a more strategic view of London health services.
Trouble shooting
At
the time of its establishment, financial growth had never been greater, but
this ended with the economic downturn. Trusts in south east London
had long-standing financial problems, recording annual deficits every year since
2004/2005 from the unaffordable and irreducible costs of its whole hospital PFI
schemes, 16% of their income. Cost-improvement schemes could not restore
financial health without risking the quality and capacity of services. In 2005 a
major review taking 5 years was established (A Picture of Health),
covering Queen Elizabeth, Woolwich and Bromley Hospitals, Queen Mary Sidcup and
Lewisham. The SHA would have liked to have examined all services
in south east London simultaneously, but this proved too difficult. The
final proposal was a large reduction in medical and acute bed capacity at the
Queen Mary’s Sidcup site with the closure of 284 acute beds and the cessation of
emergency admissions. To facilitate service changes a single
merged trust was established to cover three hospitals in 2009 with a total
combined debt of £149m. The merger was a financial failure, and the
Care Quality Commission found the trust was not complying with some standards of
safety and quality.
Strategy
Perhaps the SHA's most important action was, while Sir David Nicholson was chief
executive, to commission a clinician, Professor Sir Ara Darzi, to review
London's health care system. Darzi, intelligent, hardworking and
alert to trends had extensive support both in back office terms and from senior
clinicians. Legitimacy was established through the clinical leadership with an
extensive consultation programme, and by selecting a few priorities
to be tackled properly rather than trying to do everything. The
three priorities were stroke, trauma, and the
polyclinic programme. The course and outcome of this programme were subsequently
reviewed by its key officers.22 Darzi’s first
report The Case for Change (March 2007) argued
that the current system was wrong because it could not handle
health inequalities, patients' expectations, the need to centralise specialised care,
the relationship with academic medicine or give value for money. A
Framework for Action was published in July 2007, days after
Darzi’s ennoblement and his appointment by Gordon Brown as a junior health
minister in the Lords.
Darzi was one of the "goats" in Brown's "government of all talents”, and
he came to believe that his appointment as a Labour Minister turned people
against his report, though it was the product of many hands including
McKinsey’s.25 It recommended 5 principles, an individual
focus on patients' needs, services local where possible and centralised where
necessary, focus on health inequalities, prevention rather than cure and truly
integrated care. Technical groups had looked at population trends, e.g. the
population expansion in the "Thames Gateway", and the likely health
problems in London over the coming years. Clinical working groups
considered appropriate policies for care and the care pathways best suited to
differing groups of patients. Hospitals might be classified as
local hospitals, elective centres with high throughput, major acute
hospitals handling complex work, specialist hospitals, and academic
health science centres.
Brilliant in conception, but according to the Guardian a
recipe for turbulence, it was a blueprint for a radically different NHS. Darzi
envisaged that London primary care would be provided by 150 polyclinics,
handling much work previously undertaken in hospitals. Some large practices
already provided extensive facilities but the inclusion of imaging, consultant
outpatient sessions, and minor surgery would require much
investment. The number of major acute hospitals would be cut by more than a
half, some being restricted largely to cold surgery. There might
be some 12 specialist hospitals and 8-16 major acute hospitals. Patients
in emergencies would be admitted to the hospital best suited to their needs;
near or far. Services for the mentally ill and long-term conditions
needed improvement, and the report was fleshed out with reports of
working parties, for example on maternity services.
For maternity, a
tiered system was proposed according to the clinical and social
need of home delivery, midwife-run maternity units some on a
hospital campus, and full-scale obstetrician round the clock
hospital units. Darzi seemed to believe that the health service would be rebuilt
starting from scratch. The costings provided by McKinsey's
attracted significant criticism. Major savings depended on the
ability to transfer services into the community, but some polyclinic schemes
seemed lavish and were likely to cost and not to save money. Darzi accepted that
the plan had a long timescale and was confident that he could take others with him, but
this was only partly true. He wished his concepts to influence national thinking
particularly on quality, but he offended some by offering instant solutions to
problems with which people had wrestled for years. The SHA went to publicconsultation, and
a bare majority accepted most of the proposals. A joint committee of primary
care trusts (PCTs) accepted the proposals in June 2008.
Trauma and Stroke reconfiguration
NHS London hosted Healthcare for London, a transient organisation paid for by the 31 PCTs to encourage planning of the most complex services London wide. Already heart attacks had been centred on four key hospitals. From 2006 NHS London consulted on and implemented reconfiguration of major trauma and acute stroke units. It sponsored the work that established a ‘case for change’; usually led by a clinician from the field and a steering group
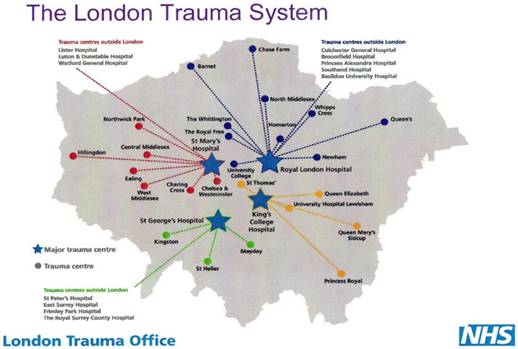
reviewing the evidence. This was not always hard or absolute but
in general suggested that the more acentre did, the better they
were at it. Economic arguments were not paramount. The
decision about how many centres there would lie largely
with NHS London and the expert group and might be contentious. Similarly,
the expert group decided on the criteria by which applicant trusts would be
judged for centre status. Trusts submitted their bids, NHS London
evaluated them and once decided, the commissioning process was used to cement
arrangements. Against much opposition but usually with strong clinical support
specialist care was centralised. Many opponents of the proposals
were converted. In February 2009 eight hyperacute stroke units (HASUs) and four
trauma units were established. As a result of stroke
reconfiguration, virtually all patients who would benefit from thrombolysis got
it (18%), three times more than in the country as a whole, saving some 400 lives
a year. The HASUs were The Royal London Hospital, St George’s
Hospital, King’s College Hospital, Northwick Park Hospital,
Charing Cross Hospital, University College Hospital, The Princess Royal
University Hospital and Queen’s Hospital Romford supported by 24 stroke units
where patients would continue their recovery.
Post Darzi Reconfiguration in London
To
aid reconfiguration, in 2009 the Primary Care Trusts created five subgroups,
three north and two south of the Thames later followed by more formal
merger of the PCTs. Reconfiguration proposals were developed in North East
London and North West London (the Barnet, Enfield and Haringey
Clinical Strategy) but stalled. So did the strategy for the south west, Healthcare
for South West London. A delay imposed by Andrew Lansley
on taking office as Secretary of State for Health provided opponents of local
change with ammunition. The polyclinic programme,
itself essentially based on proposals already in hand, was ended but the primary
care trusts and their successor clinical commissioning groups pressed on with
rational developments under the banner of integrated care to improve services
for the frail elderly, with its increasing incidence of long-term problems. Evaluation showed
little evidence that the polyclinic programme had
improved service development, access, quality of care and patient experience,
and it had not generated significant cost savings. Clinical
pressure continued to ensure service transformation in cardiovascular, cancer,
mental health, maternity and neonatal intensive care and paediatric services.
A major reconfiguration in North West London, Shaping a
Healthier Future, was approved, enabling the closure of A and E at Charing
Cross, Central Middlesex Hospital, and Ealing in October 2013.
Biomedical Research
Centres (BRCs) and Academic Health Science Centres (AHSCs)
Since the time of William Osler and the Flexner report a century previously there had been recognition that service, teaching and research were mutually supportive. Driven from a research standpoint by Dame Sally Davies, the UK government recognised the economic, financial and clinical advantages of backing medical developments, research leading to better treatment. The example of major biomedical research centres in the USA, which had spearheaded clinical development, led to the establishment of the National Institute for Health Research (NIHR) and consideration of which centres should be supported to encourage "translational research". A panel of international experts chose centres in open competition as world class in research. In December 2006 Patricia Hewitt, the Secretary of State, announced five multispecialty trusts that would be supported, three in London (Kings, UCLH and Imperial) plus Oxford and Cambridge, and a further six in particular clinical fields. NHS research moneys went preferentially to these power houses of translational research.
2010. The Coalition and the Health and Social Care Act
Labour was defeated in the 2010 election and the new Secretary of State, Andrew
Lansley, arrived with further proposals for reorganisation that he
had published while in opposition. Lansley was distrustful of
central planning. He immediately moved to embargo proposed reconfigurations,
imposing new criteria such as local support from the public and general
practitioners. Because the London SHA had been in advance of other
authorities, it was particularly affected by this decision and important
strategic plans were placed at risk. The Chair, Sir Richard Sykes,
previously chief executive of GlaxoSmith-Kline, resigned believing that the
delay was driven politically and not by logic. Many of the
reconfiguration proposals such as those in North East London had emerged from a
long process of clinical involvement and public consultation. Others, as at
Chase Farm, were necessary and had been delayed for years by political and
public dissent. While some could be criticised, such
as the belief that polyclinics would move up to half acute care into the community,
saving money, to delay restructuring at a time of financial crisis was
questionable. Many of the trusts where restructuring was planned had financial
problems and were also at risk of providing poor care. NHS London considered how
mergers might assist.
The White Paper, Equity
& Excellence, Liberating the NHS was followed by compromises
within the coalition, fierce political battles and following the Health and
Social Welfare Act (2012), major organisational change.20 In
2013 the London SHA and Primary Care Trusts were abolished, to be replaced by a
London regional branch of NHS England with three area groups, two north and one
south of the Thames. Pan-London planning and hospital reconfiguration
became more difficult. Commissioning functions were transferred to
clinical commissioning consortia, and lines of accountability were
confused. Within a year nobody could be found willing to defend the changes that
were generally held to be mistaken. When appointed as Chief Executive of NHS
England in 2014, Simon Stevens was left to try to sort out the mess without
resorting to further legislation, against a worsening economic background.
Because of the
economic outlook, McKinsey was commissioned in 2008 by the
Department of Health to examine NHS finances. Its report in March 2009 suggested
the need for swingeing economies. The NHS Chief Executive said that efficiency
improvements of £15-20 billion would be required in the three years between 2011
and 2014. In 2011, tariff payments were cut, and some
activity was restrained, most acute trusts in London projecting an in-year
deficit of 6-9%. Monitor found that most trusts not yet of
foundation status were financially at risk. Some such as the Royal
London were burdened by major PFI commitments (10% of the entire hospital PFI programme)
that debarred it from meeting tests of financial stability. Others
had historical debts. NHS London confirmed that
Newham, Whipps Cross, North West London Hospitals, West Middlesex, Barnet
and Chase Farm, St George’s Healthcare, South London Healthcare, and Barking,
Havering and Redbridge Hospitals would all remain in deficit in the medium term.
In April 2011 Imperial College Health Care Trust, budget £910 million, had a
deficit of £40 million, and the Chief Executive and Finance Officer resigned. The
SHA rightly believed that if acute trusts were left with their levels of
deficits, London would end up with failing trusts with significant debt, which
would result in performance failure, not only financially, but in patient care.
The Francis Report (2012) following the problems at Mid-Staffs had made clear
that good care depended on safe nurse staff levels. Pressure to recruit added to
financial problems, and conversely several trusts with poor staffing and bad CQC
reports went into 'special measures.' In 2011 NHS London examined
the financial viability and clinical sustainability of the 18 acute NHS Trusts
in London yet to achieve Foundation Trust status. (Safe and Financially
Effective - SaFE). Even assuming major improvements in productivity, only a
third would be in a viable long-term financial position by 2014/15. In
2013 NHS London was abolished and responsibility for strategy passed to the new
Clinical Commissioning Groups (CCGs) which formed a London wide Clinical
Commissioning Council, to the London regional office of NHS England, to Monitor
for foundation trusts, and the Trust Development Authority (TDA) for other
trusts (two organisations amalgamated in 2016.)
Merger, at least for the Southeast London Healthcare Trust, was not
a panacea. 24 In 2012 the Secretary
of State placed the trust into administration. Faced with a rising deficit
an administrator was appointed by the Secretary of State in 2012 who later
approved his recommendations. Among them was the closure of the A and E
department at Lewisham, but this went to Court, and it was ruled
that it was outside the remit of the SOS for this to be done. In October 2013
the Trust was dissolved, and in its place a new trust (Lewisham and Greenwich)
managed QE Woolwich and Lewisham hospitals; King's College Hospital FT took Princess Royal
Bromley; and Oxleas FT Queen Mary's Sidcup. The
DoH paid the excess costs of the PFI buildings and wrote off debts so that the
new organisations were not saddled with historic deficits. Time
had been lost and local staff traumatised.
Seeking solutions led to other risky decisions. The merger of
Barts, the Royal London, Whipps Cross and Newham was agreed by the Secretary of
State (2012). Within
a year the merged trust was in "financial turnaround”,and in 2015
the Chair, Chief Executive, and Chief Nurse resigned. The hospital went into
"Special Measures" because of its continuing deficit (£93 million) and poor CQC
reports.
In
North West London McKinsey's were asked to examine the configuration of
services, an exercise that was expanded and led to consultation by the new CCGs
on 'Shaping
a healthier future' in
2012 that proposed a reduction in A & E units coupled with attempts to improve
services in the community.
Several London
trusts were placed into Special measures for either quality or financial
reasons, or both. Trusts affected were Barking, Havering and Redbridge
University Hospitals, Barts Health NHS Trust, Colchester University Hospital NHS
Foundation Trust ,Medway NHS Foundation Trust and St George’s Hospital NHS
Foundation Trust
Improving health and health care in London
In December 2011
the King's Fund also took stock of the financial and policy landscape, the
successes and unfinished business of Darzi and Healthcare
for London, and the loss of momentum through the decision to abolish the
SHAs in London as elsewhere.21 Its assessment was updated in
2013 listing significant reconfiguration developments. A common theme was
the aspiration to develop more integrated care, particularly in primary and
community settings, 21 though this had
never shown to save money.
The financial situation, though dismal, was at least clear. It was policy that was uncertain. The Fund thought that London, with a greater concentration of problems and financial difficulties than elsewhere, faced a strategic vacuum with no clear lead to coordinate services and drive through necessary changes. Much had been accomplished in heart disease, stroke and trauma by having a central focus. Only 16 of 42 London trusts were currently foundation trusts, with around half of the remainder unlikely to be financially viable in the medium term. The Fund saw a reduction in the number of hospitals and the resultant political conflicts as inevitable.
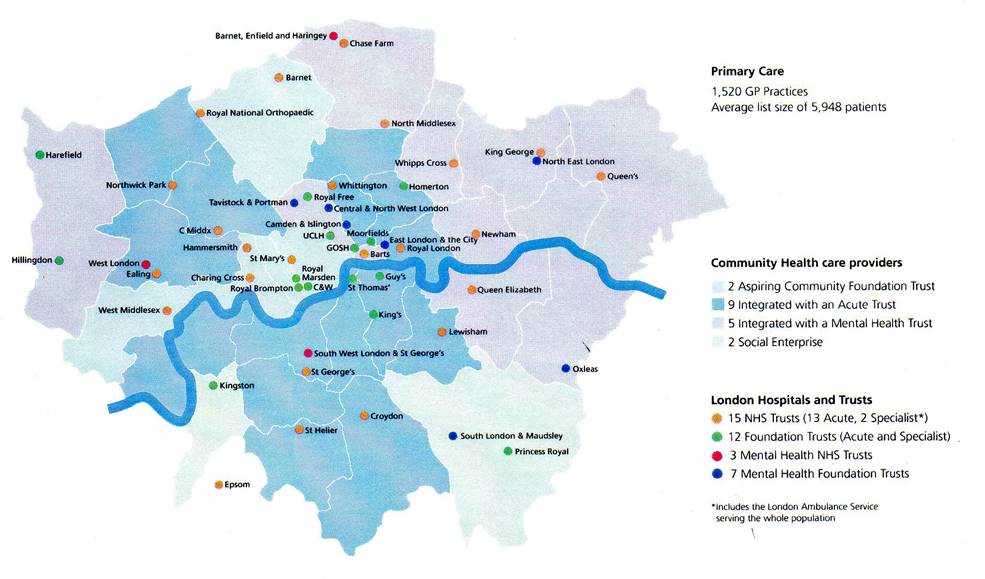
NHS England
London Region published ‘London
- A Call to Action’ in 2013, which like the Darzi reports aimed to
stimulate debate about the challenges faced by the NHS in London and the case
for "transformation.". A useful guide, the challenges were
presented better than the possible solutions.26
The Academic
Health Science Centres were now playing a role in reconfiguration. For
example, it was agreed that specialist cardiac services should move from
UCLH to Barts, creating the largest centre in the country, while specialist
urological cancer surgery would transfer to University College London Hospitals. UCL
Partners described the move as a “once-in-a-lifetime opportunity” to create
world class cancer and cardiac care for 6 million people in London and beyond,
on a scale similar to the reconfiguration of stroke care across London.
UCLH said there were only two things it could do at world-class standard, neuroscience, and
cancer. "It's not possible anymore for everyone to do everything.” The
concentration of expertise allowed Barts to compete with international
cardiac centres, such as the Cleveland Clinic, while UCLH competed
with the equivalents for cancer, forexample, the Memorial
Sloan-Kettering cancer centre in the US.
The return of a
Conservative government with a modest majority did not lead to immediate change.
Indeed the previous Secretary of State for Health, Jeremy Hunt, retained his
position. The immediate problem was mitigating the problems that had been
created by the Lansley reforms, without further legislation, and at a time of
almost an unparalleled economic crisis.
A plethora of authorities and bodies had made administration, let alone management and planning difficult.
The complexity of the changes in 2013, and the processes now to be gone through seemed massive, according to Ruth Carnall, retiring chief executive of NHS London.22a NHS England moved slowly to remedy matters. Monitor, which dealt with Foundation Trusts, and the Trust Development Authority concerned with the rest, were merged in 2016.
In 2014, against
the background of falling resources and fragmented commissioning
responsibilities, The NHS five year forward view was
published, emphasising prevention, integration of services and
putting people in control of their health. It described new care models; most
involved closer relationships between providers, NHS Trusts, and
Local Authorities, stressing collaboration rather than competition. The two
principles now appeared to be working together, rather than
competition, and a move towards integration of health and social services to aid
the care of the elderly and those with disabilities and long-term problems. Subsequently, Sustainability
and Transformation Plans (STPs) were developed, concerned with
health, care, and financial stability. Forty-four
'footprints' were defined; coterminosity was not generally
attempted, and they varied vastly in size. The five covering London
reflected the Turnberg sectors; the areas and local leadership were often
determined centrally. There
had been limited public involvement in
the process , but there had also been limited involvement of GPs and Local
Authorities in some areas. STPs had no legal framework or formal accountability.
The emerging plans and the financial costing were ‘high level,' often with little indication of specific changes in the services although the financial crises might drive the incorporation major changes. The assumptions made in some areas might not stand scrutiny, and many were dependent on taking beds out of the system, or on capital spending. The requests from London trusts were substantial.
In November 2017 a Memorandum of Understanding was signed y the Department of Health, the Mayor of London and london authorities, and NHS organisations, pledging to work together "to test opportunities to transform health and wellbeing outcomes, inequalities and services in London through new ways of working together and with the public, through a programme of collaboration and co-development with the five London devolution pilots."
Inner London
Trusts and Foundation Trusts as of 2016
Structurally, the financial climate had encouraged organisational mergers. Larger Trust groupings appeared in four of the five Turnberg sectors
Dates of joining
the trust and of foundation trust status.
North East London
Barts Health NHS
Trust (Trust created 2012)
The Royal London
Hospital, St Bartholomew’s Hospital, Newham University Hospital (2012), Whipps
Cross University Hospital (2012)
Homerton
University Hospital Foundation Trust (2004 FT Status)
North Central
London
Royal Free
Hospital London NHS Foundation Trust (2012 FT Status)
Royal Free
Hospital, Barnet Hospital (2014), Chase Farm Hospital (2014)
University
College London Hospital NHS Foundation Trust (1994/2004 FT
Status)
University
College Hospital & Middlesex Hospital (1982), National Hospital for Neurology
and Neurosurgery (1996), Royal National Throat, Nose and Ear Hospital (2012),
Eastman Dental Hospital (1996), Royal London Hospital for Integrated Medicine
(2002)
Great Ormond
Street Hospital for Children NHS Foundation Trust (2012 FT Status)
The Whittington
Hospital NHS Trust
North Middlesex
University Hospital NHS Trust
The Hillingdon
Hospitals NHS Foundation Trust (2011)
Hillingdon
Hospital, Mount Vernon Hospital
Royal National
Orthopaedic Hospital Trust, (Stanmore & Bolsover Street)
Moorfields Eye
Hospital Foundation Trust (2004 FT Status)
Moorfields has
many satellite units embedded in other hospitals in London and the Home Counties
North West London
Imperial College
NHS Healthcare Trust
Charing Cross
Hospital (2007), Hammersmith Hospital (2007), Queen Charlotte’s Maternity
Hospital (2007), St Mary’s Hospital (2007), Westminster Eye Hospital (2007)
Chelsea and
Westminster Hospital NHS Foundation Trust (2006 FT
Status)
Chelsea and
Westminster Hospital (Built on site of St Stephens and opened 2003), West
Middlesex University Hospital (2015)
London North West
Healthcare Trust (2014)
Central
Middlesex Hospital, Ealing Hospital, Northwick Park Hospital, St Mark’s Hospital
Royal Brompton
and Harefield NHS Foundation Trust (2009 FT Status)
Brompton
Hospital, Harefield Hospital
South West London
St George's
University Hospitals NHS Foundation Trust (2015 FT Status)
(Incorporating
the Atkinson Morely Hospital)
Kingston Hospital
NHS Foundation Trust (2013 FT Status)
Royal Marsden NHS
Foundation Trust (2004 FT Status)
Royal Marsden
(Chelsea), Royal Marsden (Sutton), Royal Marsden day unit in Kingston
Hospital.
South East London
Guy’s and St
Thomas’ NHS Foundation Trust (2004 FT
Status)
Guy’s Hospital,
St Thomas’ Hospital
King's College
Hospital NHS Foundation Trust (2006 FT
Status)
King’s College
Hospital, Princess Royal University Hospital, Farnborough Common (2013),
Orpington Hospital
Lewisham and
Greenwich NHS Trust
Queen Elizabeth
Hospital Greenwich, University Hospital Lewisham
In January 2020, reports were received from Wuhan province
in China of the outbreak of a new viral respiratory disease. It was spreading
rapidly, and while the majority of cases were mild, if not asymptomatic, after a
few days a minority developed a severe respiratory illness requiring intensive
care and often ventilation. Other
organ failures, such as renal failure, also occurred. Among these, a substantial
and increasing number died. The spread of the disease to many other countries,
aided by air transport, was rapid. By March 2020, it was recognised as an international pandemic.
Soon millions of cases and tens of thousands of deaths were being reported.
France, Italy, Spain, Iran, the USA and Britain were hard hit and vrtually no
country escaped. In the UK London was hit early, with cases in the thousands and daily deaths in the hundreds.
The government acted, pledging additonal resources to mitigate the effect of unemployment as the country closed down, and writing off many historical hospital debts. The Prime Minister, Boris Johnson, contracted the disease and was admitted for a few days to intensive care at St Thomas', and nationwide social isolation was instituted. The use of public transport fell by 95% as only key workers, NHS and food chains, remained at work. The Chief Medical Officer, Professor Chris Whitty, rapidly became a media personality in daily briefings and his Gresham Lecture. The effect on London's hospitals was dramatic. Elective admissions ceased while wards and theatres were re-purposed as intensive care units. Private hospitals such as the Princess Grace were integrated into the system, sometimes being used for urgent cases who were not infected. A new hospital was constructed within days at the Excell exhibition centre (The Nightingale Hospital) in case hundreds or thousands of intensive beds were needed, although, in the event, a massive increase in the intensive care facilities of all London hospitals managed to cope with the demands and after two months the huge number of cases in London fell to low levels. Lockdown was eased and a further massive surge in cses was the result. Lockdown was reinstituted.
Some types of care, for example, cancer care, were
centralised at the Royal Marsden to avoid infection, while other hospitals
became temporarily single specialty. NHS workers, although provided with a level
of personal protecting clothing, died in their dozens, many from ethnic
minorities. Residents of residential care homes were badly hit, the majority
recording cases. A massive
increase in testing for the virus was instituted, although iin the face of the
numbers contract tracing was initially abandonned. A rapid search for a
vaccine began, for existing drugs that might affect the
disease and technology that would improve contact tracing. .
The State of Play, 2020
Subsequently under the Lansley reforms the Department of Health stepped back from involvement, and there was a single strategic authority, or regional branch of NHS England, for London;. Ways had to be found to remedy the lack of a focus for strategic planning, NHS England encouraging the creation of ‘Sustainability and Transformation Plans’. By 2020 there were hints that that these and "integrated care organisations" not only aimed to increase cooperative working, but might come to resemble the previous regional authorities.
The medical
schools had sorted out their problems. Academic
Health Science Centres were flexing their muscles, but
the gospel of competition was giving way to collaboration, not only
within the NHS but with local authority social sevices. Planning
for services such as heart and stoke was taking
place across the
metropolis, rather than within individual hospitals, with substantial clinical
involvement, and driven by commissioning. Increasingly the burden of care of the
elderly and those with multiple problems was leading to "integrated care" with
attempts to unite the work of general practitioners and hospital services.
The problems of developing, and where necessary remodelling, London
in matters of health administration "is admittedly one of unending difficulty."
So said The Lancet in 1920, and when this book was first published in 1986 few
could have predicted the pattern of London health services and hospitals three
decades later.
Advance was coming from success in working with clinicians, whether
consultants or GPs. The attempt to predict the future at this juncture would be
equally silly. The trend to look at clinical services for quality and cost
across hospitals and trusts is encouraging. London remains, however, with its
hospitals, universities and academic health science centres a
powerhouse of talent. Long may it remain so, a wild problem but, again in the
words of The Lancet on 18th January 1873, "a
service doing on the whole an enormous amount of good and
necessarily doing also a certain amount of mischief."
1 Greater London Authority. London’s
Changing Population. DMAG briefing 2005/9 & 2005/17. 2005.
2 London Health Planning Consortium. Acute hospital services in London. London: HMSO, 1979.
London medical education. A new framework. Report of a working party on
medical and dental teaching resources. (Chairman: Lord
Flowers.) London: University of London, 1980.
3 Department
of Health. Report of the inquiry into London's health service,
medical education and research. (Chairman: Sir Bernard
Tomlinson.) London: HMSO, 1992 and Response of the Department of Health. Making
London Better. London: HMSO, 1993.
Gorsky M, Preston V. The Tomlinson Report and After. London
School of Hygiene and Tropical Medicine, Witness Seminar, November 2012.
4 Health
Services in London – a Strategic Review. (The Turnberg
review). London. Department of Health. 1997.
5 NHS
Management Inquiry. Letter dated 6 October 1983 to the Secretary of State,
Norman Fowler, from Roy Griffiths, Michael Betts, Jim Blyth and Sir Brian
Bailey.
6 Parliament. Working
for patients. Cm 555. London: HMSO, 1989
7 Enthoven
AC. Reflections on the management of the NHS: an American looks
at incentives to efficiency in health services management in the UK.
London: Nuffield Provincial Hospitals Trust, 1985.
8 Dorrell
S. The Millennium lecture. Manchester Business School,
1996
9 The
new NHS - Modern, Dependable, Cm 3807, Department of Health, London, 1997
10 Parliament, The
NHS Plan – a plan for investment, a plan for reform, Cm4818, London, 2000.
11 Primary
Health Care in inner London (the Acheson report) (1981)
12 Parliament. Promoting
better health, the government’s proposals for improving primary health care. CM249
London. HMSO. 1987
13 Parliament NHS
Plan – a plan for investment, a plan for reform. Cm 4818, London 2000
14 The
provision of Acute Hospital Services,. London, RCS 1998
15 Cuts
and excellence [leading article]. BMJ 1982; 284: 294
16 London
health care 2010 : changing
the future of services in the capital. King
Edward's Hospital Fund for London. King's Fund Commission on the Future of
London's Acute Health Services, 1992
17 Great
Britain, Ministry of Health and University Grants Committee. Postgraduate
medical education and the specialties (with special reference to the problem in
London). (Chairman: Sir George Pickering). London, HMSO, 1962.
19 A
Framework for Action. Healthcare for London (NHS London) Lord
Darzi. London 2007
20 Equity
and Excellence - Liberating the NHS. White Paper July 2010
HMSO Cm 7881
21 Improving health and health care in
London. King's Fund, London, 2011.
Leading Health
Care in London. Ham C, Nigel
Edwards N, Brooke B. King's Fund. London. 2013
23 The
Lancet, 14th August 1920.
24 Parliament 2013 Securing sustainable NHS services: the Trust Special Administrator’s report on South London Healthcare NHS Trust and the NHS in south east London.
25 The
Wisdom of the Crowd. 65 views of the NHS at 65.
(Ed. Nick Timmins) London. Nuffield Trust, 2013.
26 London:
A Call for Action. NHS England, London Region, 2013.