|
The embarrassing position of London in matters of health administration has always been recognised by those who study local
organisation, and the problems of developing, and where necessary remodelling, that administration, when the health of so vast and
heterogeneous a population is concerned, is admittedly one of unending difficulty.'
The Lancet, 14 August 1920
Few things in the hospital world are accidental, and virtually nothing in London is the result of chance. This book is the outcome of curiosity about why things are as they are. A capital city is often the centre of political, ethnic and sociological changes and the hospitals which are maintained by such a society must in some measure reflect the alterations taking place outside their walls. Hospitals are therefore never static, and neither is the system of which - sooner or later - they form part. London’s hospitals have been affected by changes in the population structure, the city’s politics, the development of medical science and the conquest of diseases. Professor Brian Abel-Smith has written about the development of British hospitals in a national and sociological context.1 Here the aim is more limited, to consider how during the nineteenth and twentieth centuries the hospitals of inner London developed and were shaped into a system. Many of the buildings and even more of the concepts of the last
two hundred years are still with us. Those who are interested in the hospitals of London and their future cannot ignore their past.
There is a fascination in the sheer complexity of London and the hospitals within its boundaries. ‘It is notorious’, said The Lancet, ‘that the problems of London in all matters of social administration and development are different from those present in areas not so immense. Centres of population that are less widely separated into widely differing sections of wealth, status and occupation more readily conform to general schemes.’2 London was unique in its size and speed of growth, and its local government was made no simpler by the independence, power and privileges enjoyed by the vestries and the Corporation of the City of London. Faced with the near incomprehensible complexity of the metropolis, hospital reformers, campaigners and administrators might adopt symbolic, even simplistic, concepts to guide them. Centralism, voluntarism, municipalisation, cooperation or sanitation might become battle-cries. But the problems of London defied solution by formula; the inbuilt checks and balances are too great.
The state of the metropolitan hospitals
London’s hospitals were of interest to a variety of nineteenth century reform movements. All was not well. In 1873 The Lancet criticised hospital administration, remarking that none of the eleven largest hospitals was managed in the same way. There were three radical faults.3 First, medical staff were often excluded from the management committee, so that much was left in the dark which should have been told. Second, financial control and general administrative power might lie in the same hands, with the result that expenditure was screwed down in the wrong place and at the wrong time. Finally, the committee of management did not always have absolute control over the nursing staff.
Professional affairs also left much to be desired in the early part of the century. Looking back fifty years to its foundation, The Lancet said
`Speaking broadly, it may be said that professional knowledge was a private and individual rather than a public and widely diffused possession. The eminent men who, by dint of great gifts and unceasing labor, had come to be recognized as masters of their craft, were hindered in their desire freely to disseminate the treasures of their experience and erudition, and were so hindered partly by the absence of easy and recognized channels of publicity, and chiefly by the mistaken views of inferior men, colleagues who had been placed in hospital offices by nepotism or by payment, and who shrank, like the quacks our own day, from imparting to others the weapons by which they trusted to win a way to fortune for themselves. At that time medicine and surgery were still "mysteries", and the hospitals, their temples, were closed to all who had not paid the necessary fee, and at all periods that fee did not cover. The lectures of great men, comparatively seldom embodied in books, were indeed taken down more or less completely by some of the members of their classes, but even then they were guarded with jealous care against publication. A scientific discovery, a new medicine, a new method of treatment, or a new theory of disease, remained for months or years the property of a small number of persons, used or tested perhaps only within the walls of a single hospital' 3
Such a state of affairs could not last. From the date of the first census in 1801 there was an increasing belief that the state had a duty to know in detail the number and economic conditions of its citizens. Social knowledge of this sort came to be seen as a kind of action in its own right, and the precursor of change. Factual information about the size of a population, its death rate, the migration to the cities, the sanitary conditions of towns, and the institutional treatment of the sick paved the way for reform. Changes in the hospitals took place alongside the campaigns for parliamentary reform, developments in local government and municipal facilities, the creation of a public educational system and the great sanitary movement. Controversy and debate were characteristic of Victorian England as ‘good men’ fought against ‘vested interests’. In his book, Portrait of an Age, G M Young said: ‘I was constantly being told that the Victorians did this, or the Victorians thought that, while my own difficulty was to find anything on which they agreed.’4 So it was in London’s hospital world, as conflicts and disputes were waged in the press.
Small towns only needed one hospital, or a small number of institutions each serving a specific purpose. Capital cities like London and Paris had many and it was in the nineteenth century that it came to be appreciated that the various institutions interacted with each other as components of a system. The approach to organisation was vastly different in the two cities. In Paris the property of the hospitals had been pooled and to their income was added a large contribution from the municipal authority. The hospitals were open to all the sick poor who had a right to claim admission. Each hospital was part of a larger whole and the staff, medical and non-medical, were employed by a single authority and could be moved between institutions. This extreme form of centralism had produced an effective hospital service in Paris, albeit one which was hardly acceptable to English taste.
In London the pattern of the hospital system had grown up in a more haphazard way, shaped in part by the growth in the size and wealth of the city populations, the illnesses from which people suffered, and the advance in the capacity of doctors to treat them. In 1844 an article in The Lancet said that the entire hospital system in England was essentially bad. The hospitals were charitable institutions which could only relieve a certain amount of misery. The state contributed nothing and exercised little or no control over them. The workhouse infirmaries were the state hospitals, and such was their quality that it was distressing that the destitute, when sick, should have to take refuge in them. The Lancet preferred centralisation on the Parisian model, placing all hospitals under a central authority and the same regulations. There was little hope of this, for it would require major changes to the Poor Law and the shape of the poor law system of medical relief.
The influence of the press on hospital development was considerable. The Lancet was founded in 1823 by Thomas Wakely, a friend of the radical politician Cobbett, who was brought up in the West Country and then apprenticed to a country general practitioner. Then, following custom, he came to London to attend the Webb Street School, run by the Graingers, and to walk the wards of the Borough hospitals. The heights of the profession were not open to him as he was unable to pay to be apprenticed to a leading surgeon, and so he entered general practice with the help of his father-in-law. During a melodramatic episode in his first year in practice he was assaulted and his new house was burned to the ground. He turned to journalism and his radical views found a target in the power possessed by the elite of the hospitals and the Royal Colleges.
His journal had several functions: to work for medical reform, the abolition of quackery, the rights of the rank and file, and the education of the profession. Few doctors, after qualification, could either afford or were able to attend the practice of the hospitals, so fought for a free medical press and the right to publish medical and scientific lectures, previously regarded as the private property of their author. While editor of The Lancet he fought parliamentary elections and eventually entered the house as a radical member, where he pressed the case for medical reform. He also became one of the first medical coroners.
Wakely’s campaigns sought to force hospitals to improve their management, for he opposed nepotism in the selection of medical staff and the systems of closed government as adversely affecting the care of the poor and the education of students.
6 He reported the decisions taken in the hospitals and the views he expressed were always forthright and sometimes libellous. His accounts of hospital affairs were widely read and at sixpence a copy The Lancet became a prosperous venture. Not surprisingly Wakely encountered great opposition and was frequently in the courts, but when the Charity Commissioners enquired into the endowed hospitals of St Bartholomew’s, St Thomas’s and Guy’s they said that the publicity the ‘greater operations’ were receiving was ‘highly advantageous’ for it made the surgeons exert themselves to the utmost.7The emergence of The Lancet and other journals, some of which were founded to attempt to counter the effect Wakley was producing, was a reflection of the increasing freedom and growth of the popular press. Even the mighty Times would comment upon events in the hospitals. The Medical Times, founded in 1839 and sold at half The Lancet’s price, also sided with the reformers until its ownership and policy changed. The Medical Gazette, edited by Roderick MacLeod of St George’s, supported the establishment. The medical journals all adopted an abrasive style, and fought each other. The Lancet maintained that it alone was independent, whilst its contemporaries were confined ‘to the narrow task of upholding particular men or parties, promulgating or supporting measures which advanced particular interests.’
Social reformers have always been part of the London medical scene, and have never had need to complain of a want of subject matter. Sometimes they mellowed with age, but they frequently disagreed with each other as much as with those who supported the status quo. Some might be involved in a number of campaigns. Edwin Chadwick, a disciple of Jeremy Bentham and a liberal by inclination, was an assistant commissioner for the enquiry into the poor law, and the Report of the Royal Commissioners (1834) was drafted mainly by him. Later he became Secretary to the Poor Law Commissioners, and was involved in central government’s reorganisation of the older system of relief. It was largely his work which led to the first Sanitary Commission in 1838 and the great Inquiry into the Sanitary Conditions of the Labouring Population of Great Britain in 1842. A key figure in the sanitary movement, he laid down precise rules for the construction of dwellings and hospitals. In his later years he was a close associate of Dr Southwood Smith of the London Fever Hospital and an adviser to Florence Nightingale. The statistician William Farr (1807-1883) was another reformer who in his earlier years provided an intellectual leadership to disgruntled members of the medical profession. Even some of Thomas Wakley’s early opponents, like Mr Guthrie, the President of the Royal College of Surgeons, were keen to raise standards and brought about change in their own organisations.8
Political and religious differences might determine who supported whom, and the governors of the great London hospitals might be either Whigs or Tories; both parties introduced measures designed to improve the hospital services. Those supporting the hospitals might be high in the church, members of the nobility, utilitarians, humanitarians, dissenters or radicals. They acted with varying degrees of enlightenment or self-interest, often inheriting their beliefs from those who had gone before them. Most came to have the same general objectives, the relief of the sick poor, the strengthening of the hospitals and higher professional standards. The majority wished to raise the poor to honest independence, although some rejected the charitable principle believing that the working man could, if properly organised, provide for his own care through provident societies. All kept a wary eye on costs and came to regard inadequate care as a scandal, whether it was a pauper dying in a workhouse or a newly qualified doctor turning a patient away from a hospital. ‘It is organisation, not destruction, at which we would aim’ said The Lancet.9 Nevertheless reformers spoke bluntly, and in the rough and tumble of the times referred to the Society of Apothecaries as Rhubarb Hall and the Royal College of Surgeons as the Bat’s Cavern.
The centre of town, where the hospitals were clustered, had long been an unhealthy place as the bills of mortality showed. Crowded conditions, great poverty, old buildings in narrow courtyards, inadequate drainage and poor water supplies were ever present, and Chadwick pointed to the association of epidemic and endemic diseases with ‘atmospheric impurities produced by decomposing animal and vegetable substances, damp and filth, and overcrowded conditions’.10 The Health of London Association believed that an immense amount of sickness was caused by defective drainage and sewerage, the shortage of pure water and inadequate cleansing of the streets.11
A greater interest in statistics and improved registration of deaths increased the information available about the diseases affecting the population. The Statistical Society of London was founded in 1834, and Farr’s work at the General Register Office with the Weekly Reports for the metropolis demonstrated differences in mortality. In 1847, the year before John Simon was appointed as Medical Officer to the Corporation of the City of London, Hector Gavin, a lecturer on forensic medicine at Charing Cross, wrote that there was an excessive mortality in town compared with the country, in some towns over others, and in some parts of the same town over other parts.12 He pointed out that the excess mortality fell mainly on the lower classes and presented the average age of death by borough. In Southwark the average age of death was 20 years for artisans and 46 for the gentry, well below that of their country cousins. London was the supreme example of Disraeli’s ‘two nations?. Patterns of disease, of life and attitudes, separated East End and West End. What reason had the west-ender to visit the east, and what advantage befell the east-ender who went up west? The populations knew little of each other’s worlds.
The pattern of disease in the capital was dominated by fevers and was associated with poverty, hunger, vice and dirt. The hospitals by themselves could do little about the underlying problems, which were attacked by the sanitary reformers. Hospitals and workhouses contented themselves with dealing with the consequences of the conditions around them; hospitals for those who were proper objects of charitable relief and the workhouses for the destitute. ‘It is notorious’, said The Lancet, ‘that the great majority of acute illnesses of the poor are directly caused, and that the residual minority are greatly aggravated, by conditions arising out of the utter neglect of sanitary legislation.’13 The need for radical reform of local government in London, with its seven different commissioners of sewers, a hundred different paving authorities, and its competitive supplies of unfiltered river water was appreciated by reformers like Chadwick. There was no coordinated approach to the problems until the Metropolitan Board of Works was established in 1855, and not until 1889 was the London County Council formed, well after the corporations of the provincial cities had been established. The twenty eight London boroughs did not replace the vestries for a further decade.
The correlation between poverty, overcrowding, poor sanitation, disease and infant death was increasingly recognised. From 1857 Dr George Buchanan, Medical Officer of Health to St Giles’ and St George’s Bloomsbury, recorded in his Annual Reports the different incidence of disease in the slums and in the better parts of his district. Five times as many infants died in the slums.14 In 1928 two Ministry officers, reporting on the institutional treatment of London’s sick, could still point to a relationship between overcrowding and the number of people receiving institutional relief.15
Demand for care was greatest where housing was poorest, and discrepancies in the correlation were mainly due to local practices. Lewisham had a good reputation and many sought care, while the board of guardians of Islington were strict in applying the criteria for admission, so fewer received indoor relief. In 1945 the London Hospital Survey again pointed to the effect of environment on the demand for hospital services, stating that ‘it seems broadly probable that the needs for an urban area like London are greater than a rural area like Dorset, and those of the east end of London greater than those of a sea-side resort like Eastbourne.’16 Census information repeatedly shows that there is a consistently high level of deprivation in inner London, which is amongst the most deprived areas in the country, and the tendency of boroughs to maintain the same characteristics over a period of many years.
London began to grow quickly during the eighteenth century. Successive maps demonstrate the speed of growth, for as late as the first half of the nineteenth century fields surrounded Islington, approached Westminster and were close to the south bank of the Thames. As the population grew new hospitals were founded in increasing numbers; St George’s in the west (1733), the Middlesex in the north (1745) and The London in the east (1740) were built on the edge of town where land was most easily available. Workhouses and infirmaries were also built on the periphery, soon to be engulfed as London grew. The demographic changes were charted by the censuses and the pattern of development was soon recognisable. Population projections appeared in The Lancet as early as 1867.17 By 1889 the journal was commenting on the high rate of increase in the outer suburbs.18 From 1871 onwards the central districts lost population in every decade, the inner boroughs reaching their peak population before the outer ones, Westminster before Hackney. Greater London expanded at the expense of the inner city, for while many still came to live in the centre a greater number were leaving to live in the suburbs (see below).
  |
The population of London, 1801- 1981
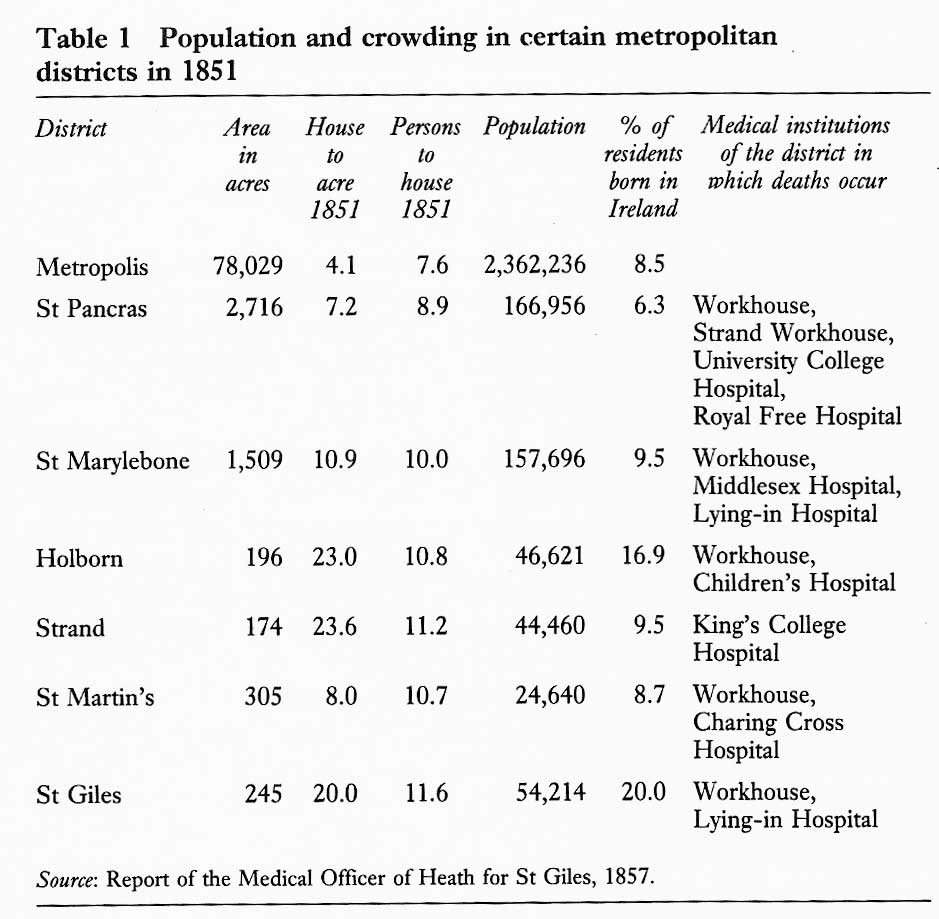
From the l830s the development of railways and the construction of new roads led to the destruction of slum property and the eviction of the poor in their thousands. After the formation of the Metropolitan Board of Works in 1855 the process of ‘metropolitan improvement’ proceeded rapidly.19 New Oxford Street and Victoria Street had already cut through massive areas of slums. Holborn, Clerkenwell Road, Shaftesbury Avenue and Charing Cross Road led to the demolition of a bewildering maze of streets and narrow alleys between 1867 and 1887 (see Table 1, below). Being dispossessed, the poor fled to live amongst those equally poor in neighbourhoods like St Pancras. Efforts to rehouse those who were displaced were made by the Metropolitan Board of Works and charitable bodies like the Peabody Trust, but went only a little way towards meeting the need. No money from the rates of the richer parishes helped the parishes to which they had exported their paupers.20 Such matters were not settled on the merits of the case, but by the effects on the rates of rich and poor parishes. Rates equalisation and the advantages of a ‘common metropolitan fund’ were frequently discussed, but how could rich and poor vestries agree on this?
The suburbs were hailed as a possible answer to the housing question. Speculative building and transport links led to rapid development, but this was not evenly spread around London. As early as 1873 tramlines spread out from Aldgate and Whitechapel to Stratford, Hackney and Stoke Newington. Other lines connected Finsbury Square to Highbury, Holloway and Archway. The introduction of cheap workmen’s fares under the Cheap Trains Act (1883), particularly along the lines of the Great Eastern to Stamford Hill, Edmonton and Tottenham, led to further speculative development. Hospital provision was never adequate in the new areas, although in total the number of beds provided in hospitals and infirmaries rose rapidly.21 The disparity between the population and the services available to them has remained a characteristic of the suburbs.
The shape of the London hospital system has also been affected by developments in medical science and medical education. In many ways it has been the activities of doctors which have determined the pattern of the hospitals. The increasing ability to treat disease and improved standards of care shortened the time patients spent in hospital, raised the demand for services and led to an escalation of cost. The development of specialisation led first to the development of the special hospitals and later to special departments within the general hospitals. Advances in bacteriology, biochemistry, physiology and radiology created the need for laboratory accommodation and service departments, so that hospitals no longer consisted merely of an operating theatre and a series of wards. Sub-specialisation ultimately meant that services had to be organised on a regional basis and the very reputation of the capital’s doctors affected the number of patients to be seen. The hospitals of central London have long served a population much larger than their local residents.
It is against this complex background of population movement, poor social conditions, disease, wealth and poverty, professional expertise, critical comment and publicity that the London hospitals developed. A complex institutional pattern emerged. Voluntary hospitals grew up beside the ancient royal and endowed hospitals. A local government service providing institutional care for sick paupers developed alongside the hospitals. A network of fever hospitals, scientifically planned from the outset, was established. Physically near to each other, staffed by doctors who had trained in the same hospitals, and often serving the same people, the different objectives and status of the institutions led them to work in virtual isolation from each other. Each hospital had its own traditions and nobody standing in the middle of a ward could have doubted for a moment the type of hospital he was in. Countless details gave each an atmosphere of its own, and the different methods of administration and levels of staffing set them apart.
References
1 Abel-Smith B. The hospitals 1800-1948: a study in social administration in England and Wales. London, Heinemann, 1964.
2 The future of the voluntary hospitals. Lancet, 1920, i, pp 613, 719, 873.
3 1823-1873 and hospital administration. Lancet, 1873, i, pp 18-20.
4 Young G M. Victorian England: portrait of an age. Oxford, Oxford University Press, 1953.
5 Comparative organisation of English and foreign hospitals. Lancet, 1844, i, p 286.
6 Causes of the depressed state of the medical profession. Lancet, 1832-3, ii, p 88.
7 Charity Commissioners. Report of the Commissioners for Inquiring into Charities. Session 16 January - August 1840, Vol 19, Part I. London.
8 Great Britain, Parliament, House of Commons. Report of the select committee on medical education and the practice of the medical profession. London, 1834.
9 Sanitary commission for investigating the state of the infirmaries of the workhouses. Lancet, 1865, ii, p 14.
10 Collins W J. The life and doctrine of Sir Edwin Chadwick. Lancet, 1924, ii, p 831, p 882.
11 Health of London Association. Report on the sanitary condition of the metropolis. London, Chapman Elcoate and Co, 1847.
12 Gavin H. The unhealthiness of London. London, J Churchill, 1847.
13 The prospects for poor law reform. Lancet, 1869, i, p 17.
14 Buchanan G. Sanitary statistics and the work in St Giles, 1857-1866. London, Various publishers, Bound copy in DHSS Library.
15 Meredith Richards and Manby. Report on the institutional treatment of the sick in London. London, Ministry of Health, 1928.
16 Gray Sir A M H and Topping A. The hospital services of London and the
surrounding area. London, HMSO, 1945.
17 Growth of London. Lancet, 1867, i, p 342.
18 The future population of London. Lancet, 1889, ii, p 80.
19 Wohl A S. The eternal slum. London, Edward Arnold, 1977.
20 Lancet, 1868, i, p 291-2.
21 Pinker R. English hospital statistics 1861-1938. London, Heinemann, 1966.